Background: Split skin grafting (SSG) is a commonly performed plastic surgical procedure. It is done to cover wounds, defects from excision of cutaneous lesions, donor sites of Fasciocutaneous flaps. The harvest of a split thickness skin graft causes a partial thickness injury. Complete re‐epithelialization occurs in 10‐14 days, although the rate may be affected by the local wound environment. However, tissue desiccation and infection can convert a partial thickness injury to a full thickness loss.
Objectives: The purpose of the study was to determine the best method of dressing the donor site split‐thickness graft between conventional paraffin gauze dressing and collagen‐based dressings with respect to the rate of healing, pain, secretion, infection, and cost. This study was done on 60 patients who underwent split skin graft procedure.
Materials : The selected sample will be divided into two groups. The donor site dressing was done in two different ways. One was dressed with collagen sheet and the other with paraffin gauze dressing.
Results: A total of 60 patients were included in this study as per the estimated sample size. The Case group i.e., the patients for whom the STSG donor site were dressed by Collagen dressing and the Control group i.e., the patients for whom paraffin gauze dressings were used. Patients with collagen dressings are found to have only minimal to moderate pain in the entire postoperative period. In these patient’s analgesic requirement is reduced, and early mobilization can be done. This is the major advantage of using collagen as a donor site dressing. We found that collagen slightly increases epithelization, which will reduce the chance of infection saving time and resources for the hospital staff and minimizing discomfort for the patient.
Conclusion: In this study it was found that dressing the donor site for split‐thickness graft with collagen‐based dressings gave better results with respect to the rate of healing and post‐operative pain scores than conventional paraffin gauze dressing.
INTRODUCTION
Split skin grafting (SSG) is a commonly performed plastic surgical procedure. It is done to cover granulating wounds, defects arising after excision of cutaneous lesions, the release of contractures, and donor sites of fasciocutaneous flaps. Common sites for harvesting SSG are thighs, legs, buttocks, and back. Skin grafting as a reconstructive procedure has many benefits, but the harvest of split‐thickness skin graft (STSG) causes damage in epidermal and dermal layers of the skin at the donor site.
The harvest of a split‐thickness skin graft causes a partial thickness injury. Complete re‐epithelialization occurs in 10–14 days, although the rate may be affected by the local wound environment. However, tissue desiccation and infection at the donor site can convert a partial thickness injury to a full‐thickness loss.
Usually, after SSG is harvested, the donor site is covered with paraffin gauze and multiple layers of pads. Patients complain of considerable pain during the early postoperative period. Often, the pads get soaked, necessitating frequent dressings and prolonging hospital stay. Numerous dressing modalities are available for the donor site, but the ideal material remains elusive. The ideal split‐thickness skin graft donor site dressing would promote healing, cause minimal pain to the patient, prevent infection, result in minimal scarring, and be inexpensive and easy to use.
Collagen, which is produced by fibroblasts, is the most abundant protein in the human body. A natural structural protein, collagen, is involved in all three phases of the wound healing cascade. It stimulates cellular migration and contributes to new tissue development. Collagen‐based biomaterials stimulate and recruit specific cells, such as macrophages and fibroblasts, along the healing cascade to enhance and influence wound healing. Moreover, collagen‐based wound dressings are uniquely suited to address the issue of elevated levels of matrix metalloproteinases by acting as a “sacrificial substrate” in the wound. In addition, collagen‐based dressing has the ability to absorb wound exudates and maintain a moist wound environment.
In this study, we used sterile collagen sheets in wet form, of bovine origin; gamma sterilized. The purpose of the study was to determine the best method of dressing the donor site split‐thickness graft between conventional paraffin gauze dressing and collagen‐based dressings with respect to the rate of healing, pain, secretion, infection, and cost.
MATERIALS AND METHODS
The study was done on all the patients who underwent split‐thickness skin grafting procedure. Inclusion criteria were patients between the ages of 18 and 60 years. A total of 60 cases were selected as the sample size.
The selected sample was divided into two groups. The donor site dressing was done in two different ways. One was dressed with collagen sheet and the other with paraffin gauze dressing. The patients were assigned to treatment and control groups according to convenience of sampling. Donor site and thickness of the STSG were the same for all the patients.
Assessment of postoperative pain was done by the Visual Analog Score (VAS) on a score of 0–10. Pain level was recorded on days 1, 2, 3, 7, 14, and 21. Healing was documented by photographs and recorded after spontaneous epithelialization of the wound or spontaneous detachment of the gauze without any interference. If a patient developed dressing soakage in between, the dressing was changed immediately, but deeper dressing over the collagen and petroleum gauze was not opened. Standard antibiotics were given for 5 days.
RESULTS
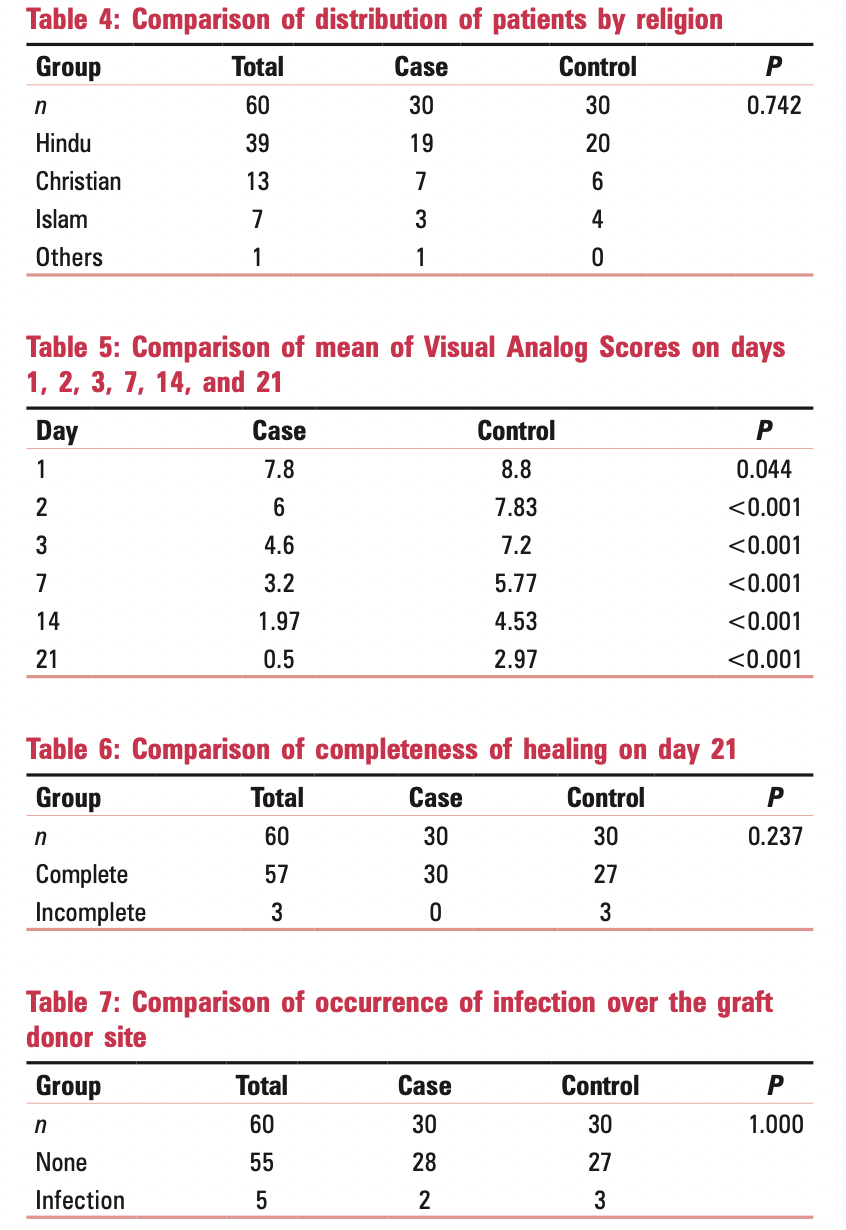
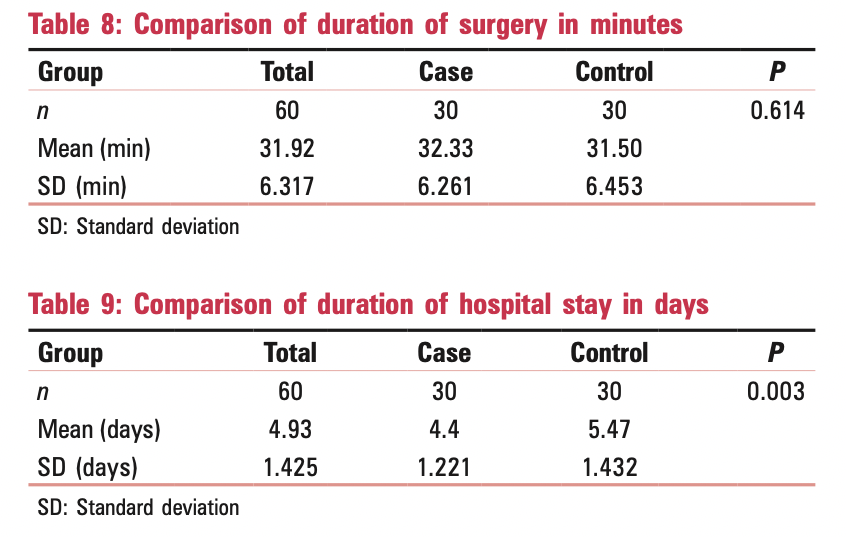
A total of 60 patients were included in this study as per the estimated sample size. The case group, i.e., the patients for whom the STSG donor sites were dressed by collagen dressing, and the control group, i.e., the patients for whom paraffin gauze dressings were used. The case group had a lower mean of VAS on all 6 days that were studied, i.e., days 1, 2, 3, 7, 14, and 21. The lower VAS scores of the case group as compared to the control group were statistically significant [Table 5]. When the graft donor sites were examined on day 21, all patients in the case group had complete healing, but three patients in the control group did not achieve complete healing [Table 6]. Five patients experienced infection in the graft donor site during the healing period, out of which two were from the case group and three from the control group. However, these differences in the completion of healing on day 21 and occurrence of infection were not significant when analyzed statistically [Table 7]. The duration of surgery for both the groups was also comparable (P = 0.614) [Table 8].
The case group had a significantly lower period of hospital stay (mean = 4.4 days) as compared to the control group (mean = 5.47 days) with P = 0.003 [Table 9].
DISCUSSION
Skin grafting as a reconstructive procedure has many benefits, including accelerating the healing of burns and other wounds and correcting scar contractures. Skin is a natural barrier that prevents the penetration of pathogens and escape of interstitial fluid. After harvesting a split‐thickness skin graft, the donor site loses its epidermis and a variable thickness of the dermis. The challenge in managing these kinds of wounds is to promote healing as quickly as possible while minimizing adverse effects and complications. If complicated by infection, split‐thickness defect may convert to a full‐thickness loss, analogous to a third‐degree burn. Of the various methods used to manage split‐thickness skin graft donor sites, none is considered as being the optimal choice of dressing. The mesh paraffin gauze dressing has for years been the primary choice of surgeons for the coverage of split‐skin donor sites, given its ease of application, conformability, low risk of infection, and minimal cost [Figure 1]. It has, however, been found inferior in many other important aspects: it is a painful, adherent dressing under which donor sites do not appear to heal rapidly. In this study, we have compared donor site treatment with the standard mesh paraffin gauze dressing and the collagen dressing. Collagen is used as a natural wound dressing and has properties that artificial wound dressings do not have. Collagen dressings can provide anti‐infective, anti‐inflammatory, antifibrotic, and analgesic properties as well as promote angiogenesis [Figure 2]. The parameters that we studied in this study were wound healing, local pain, ease of treatment, and complications.
In this study, the case group (collagen dressing) and control group (paraffin gauze dressings) were comparable in terms of patient characteristics and demographics. Pain is a common complaint after this kind of surgery and is often more severe at the donor site than at the grafted site.
The statistically significant benefits of collagen dressing over paraffin gauze for pain relief are demonstrated in this study. Dressing sites were less painful than paraffin gauze, especially after the 1st postoperative day. The case group had a lower mean of VAS on all 6 days that were studied, i.e., days 1, 2, 3, 7, 14, and 21 comparable to the study of 55 patients by Pontén and Nordgaard.
Overall wound healing, as measured by percentage of epithelialized dermis, was complete with collagen dressing than with paraffin gauze dressing. The faster epithelialization rate that had been seen with the collagen dressing can partially be explained by its physical properties [Figure 3]. Collagen, a natural structural protein, is involved in all three phases of the wound healing cascade. It stimulates cellular migration and encourages the deposition and organization of newly formed collagen, creating an environment that fosters healing because of the dressings’ chemotactic properties on wound fibroblasts. On day 21, all patients in the case group had complete healing, but three patients in the control group did not achieve complete healing. This finding is comparable to a study by Horch and Stark.[8] Five patients experienced infection in the graft donor site during the healing period, out of which two were from the case group and three from the control group. However, these differences in the completion of healing on day 21 and occurrence of infection were not significant when analyzed statistically. The duration of surgery for both the groups was also comparable (P = 0.614). The application of collagen dressing is a simple procedure and does not require special expertise.
The case group had a significantly lower period of hospital stay (mean = 4.4 days) as compared to the control group (mean = 5.47 days) with P = 0.003, probably due to decreased postoperative pain levels between the groups.
Patients with collagen dressings are found to have only minimal to moderate pain in the entire postoperative period. In these patients, analgesic requirement is reduced, and early mobilization can be done. This is the major advantage of using collagen as a donor site dressing. We found that collagen slightly increases epithelization, which will reduce the chance of infection saving time and resources for the hospital staff and minimizing discomfort for the patient.