
Abstract:
Orthopaedic-related wounds are critical situations calling for care to avoid deep infections and its consequences. The purpose of this study was to evaluate the efcacy of using honey for care of orthopaedic-related wounds with limited resources. This prospective study included 50 cases with an average age of 38.18 (range 17–63) years with 38 males and 12 females. The most frequent wound location was the leg, foot and the ankle. The aetiologies were open fractures, infected tibial non-unions, and post-operative infections. Exposed tendon was present in three cases. Bone exposure was present in two cases. Deep infection was present in 29 cases. Besides treating the primary cause, a ribbon of gauze soaked with honey was applied to the wounds after thorough saline washing. Wound sizes were variable. All cases showed improvement in all parameters with complete wound healing and full coverage of bone and tendons. Recurrence of deep infection occurred in three cases and treated by debridement. One case needed sequestrectomy of a small exposed tibial cortical fragment. Exposed tendon cases showed superfcial necrosis which was treated by simple debridement. Initial mild itching occurred in few patients with spontaneous resolution. With treating the underlying aetiology and optimising the patient’s general condition, honey was an efective, simple, and afordable method of wound care in diferent orthopaedic conditions even with exposed bone or tendons.
Keywords:
Orthopaedic wounds, open fractures, infected non-union, honey dressing , postoperative infections, ilizarov
Introduction:
Orthopaedic-related wounds are critical situations that necessitate a special care to avoid occurrence of infection and its debilitating influences on the life quality of the afected patients. Deep bone and joint infections are devastating complications which pose a formidable challenge confronted by the orthopaedic surgeons. Recognising the distinctive physiologic and anatomic characteristics of bone infections, prevention is the best course of action. Wound care is an important surgeon-dependent risk factor for infection besides prophylactic antibiotics, operating room environment and surgical technique.
Orthopaedic surgical dressings are classifed into three categories. Passive dressings (as gauze, absorbent pads and adhesive tapes) act by physical wound protection and control of exudate. Active dressings (as films, hydrocolloids, hydrofiber and foam) provide a moist environment that promotes healing and their adherence to the wound is less likely. Interactive dressings (as antimicrobials, e.g. dressings containing silver or iodine, and vacuum dressings) augment the mechanisms of wound healing.
Honey is not only a high sugar-containing solution but also a biological wound dressing having many bio-active components which can enhance wound healing by several mechanisms. Honey accelerates wound healing through actions on its three phases of infammation, proliferation and remodelling. It has antioxidant and anti infammato- ryactions. This anti-infammatory effect diminishes oedema and exudate and minimises or even prevents hypertrophic scar formation. It stimulates collagen synthesis, angiogenesis and granulation tissue formation, promotes epithelialisation, and enhances wound contraction. It reduces pain, deodorises the wounds and has a debriding action lifting the debris from the wound. Moreover, the high viscosity of honey provides a protective barrier preventing infection. Finally, yet importantly, honey has antimicrobial effects based on a multitude of factors diminishing the bioburden of wounds.
Honey had been used to treat wounds for thousands of years in multiple cultures. It was recorded in an Egyptian surgical text traced back to between 2600 and 2200 BCE. In the modern medicine, successful results have been achieved after honey application to many wounds, such as burns, different chronic ulcers, infected surgical wounds, malignant wounds, Fournier’s gangrene and neonatal wounds, along with others. The studies reporting on the use of honey as method of treating orthopaedic-related wounds are few. The purpose of this prospective study was to evaluate the effectiveness and safety of using honey as topical care for orthopaedic-related wounds with limited resources.

Method :
The frequency of honey dressing was variable according to the soaking of the dressing with exudates. This was done twice daily or once daily. With improvement of the wound condition, dressings were changed every other day. According to the culture results in infected cases, systemic antibiotics were given for four weeks.
Results:
The orthopaedic condition of cases was followed up for a mean of 33.46 (range 22–47; SD 6.61) months. Wound sizes were variable. After debridement, skin closure with wide interrupted sutures was possible in ten open fractures and seven infected non-unions, and two open Achilles’ tendonrelated wounds. Other open fracture wounds ranged from 8 to 20 cm longitudinally and 3 to 17 cm horizontally. Postoperative cases and two non-union wounds ranged from 10 to 13 cm longitudinally and 3 to 5 cm horizontally. Besides the 16 cases of infected non-unions and post-operative complications, 13 cases of open fractures were complicated by deep infection that necessitated debridement. Deep samples were taken during debridement from these 29 cases (58%) for culture and antibiotic sensitivity testing. Staphylococcus aureus was found in 12 cases (24%). Other wounds were infected by Staphylococcus epidermidis in seven cases (14%), Klebsiella pneumonia in four cases , Pseudomonas aeruginosa in four cases and methicillinresistant Staphylococcus aureus (MRSA) in two cases.
All cases showed improvement in all parameters of followup with complete wound healing and full coverage of bone (except a small part in one case) and tendons. There was improvement in the colour and progression of granulation tissue formation with gradual clearance of discharges. Contraction of the epithelialised tissue reduced the scar size. The surrounding skin remained healthy. The duration of complete wound healing since starting honey dressing ranged from four to 15 weeks according to the wound size.
Recurrence of deep infection occurred in three cases and treated by debridement with eventual control of infection. Regarding bone exposure cases, the first case showed healing of the wound with bone coverage except a small sequestered anteromedial partial cortical fragment that was excised with final dry bone coverage (Fig. 2). The second case with anterolateral distal tibial wound showed complete wound healing.
Exposed tendon cases showed necrosis of the tendon surface which was treated by superficial debridement in the clinic. Apart from these events, no remarkable side effects were recorded apart from mild itching sensation at the start of the dressing in five patients that was resolved after few days. There were no allergic reactions, secondary infections or surrounding skin complications. All patients were satisfied regarding their outcome with honey dressing.
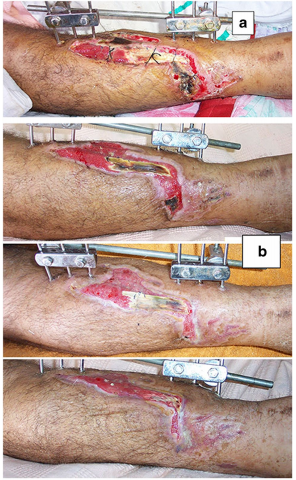

Fig. 1 A 63-year-old male patient presented with grade III-A open tibial fracture treated by monolateral external fixator. a Wound condition with tendon exposure and skin sloughing after application of external fixator. b Clinical photos with of wound healing. c Clinical photos of sound wound healing
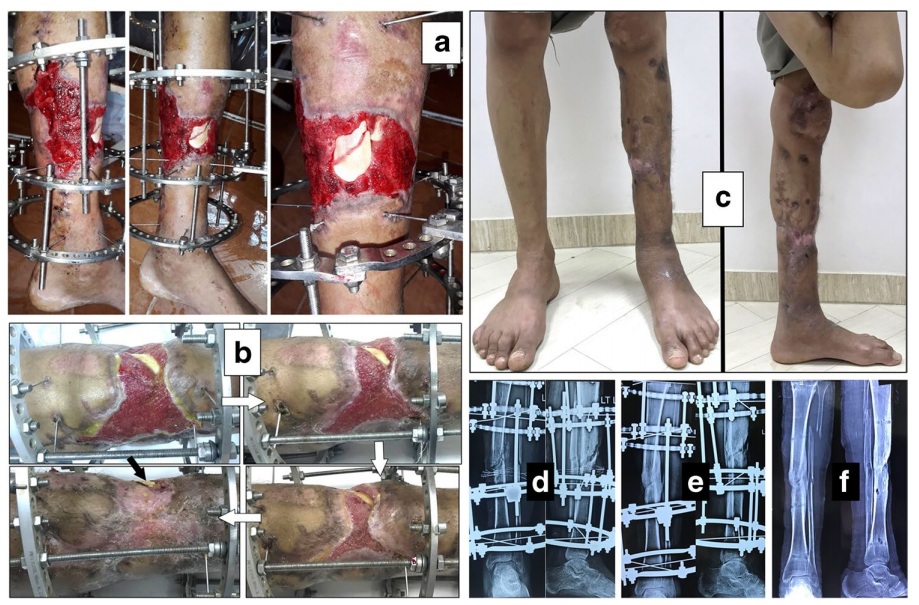
Fig. 2 An 18-year-old smoker male patient presented after previous negative pressure wound therapy that was used to treat failed rotational flap in grade III-B open tibial fracture fixed by Ilizarov external fixator. a Different views of wound at presentation with bone exposure. b Clinical photos showing progression of wound repair following the white arrow. The black arrow points to a small anterior sequestered bone fake. c Clinical photos showing the standing patient with dry scar and complete bone coverage. d, e, f Radiographs at presentation, before Ilizarov frame removal with an anterior small sequestrum in the lateral view, and after fixator removal with sound bone union.
Discussion:
The rationale for using honey in this study was the different studies conforming its positive effects on wound healing as well as its antimicrobial and antioxidant actions. Moreover, different clinical studies showed good results with different types of wounds.
A systematic review of 26 randomized and quasi-randomized controlled trials with 3011 patients having acute and different chronic wounds found that honey resulted in faster healing of both partial thickness burns compared to conventional treatment and infected post-operative wounds compared to antiseptics and gauze.
Published articles about the potential effects of honey dressings on orthopaedic-related wounds are still scarce used honey-impregnated dressings for ring fixator pin site care in 19 patients. Only two patients had superficial infection. Upadhyay evaluated the effect of honey dressing on 20 patients with traumatic orthopaedic wounds. Honey dressing only achieved excellent results in 12 cases. Four cases required multiple debridement and four patients needed local flap and skin grafting.
Besides promoting wound healing, the broad-spectrum antimicrobial effect of honey was attributed to several factors including hydrogen peroxide production, acidity, nonperoxide molecules (e.g. methyl syringate, defensin 1 and methylglyoxal) and osmotic activity. When mixed with wound exudates, honey produces low level of hydrogen peroxide which is bactericidal causing irreversible damage to the bacterial membranes, proteins, enzymes and DNA. Wounds show a biphasic response to hydrogen peroxide application. Low hydrogen peroxide concentrations enhance wound healing, but high levels delay healing. Antioxidants in honey protect the wounds from oxygen radicals which may result from hydrogen peroxide actions. Honey pH is between 3.2 and 4.5, and this acidity inhibits bacterial growth as the optimal pH of most micro-organisms is about 7.2 to 7.4 . Moreover, this acidity promotes wound healing through increasing the oxygen release from haemoglobin .
The hyperosmolarity of honey dehydrate bacteria thus preventing their proliferation or killing them. Additionally, this osmotic power draws lymphatic fluid from the wound bed and consequently enhancing the lymph outflow as in negative pressure wound therapy. This moist environment is necessary to remove damaged, dead and infected tissues. Besides hyperosmolarity, this autolytic painless debridement is attributed to the presence of the protease enzyme .
Owing to these combined actions targeting multiple and different sites in fighting bacteria, honey is effective against a broad spectrum of pathogens, including resistant bacteria and fungi. Honey is effective against Staphylococcus aureus, Escherichia coli, Pseudomonas aerugin -osa, Acinetobacter and Stenotrophomonas, MRSA, vancomycin resistant Enterococcus and extended-spectrum beta-lactamase (ESBL)-producing strains of Escherichia coli, Klebsiella species and Enterobacter species. A systematic review analysed 16 articles that included 18 diferent honey types against 32 variable bacterial species, including numerous multidrug-resistant (MDR) strains.All honey types demonstrated a high efficacy against the tested bacterial species, including MDR strains [26]. The minimum inhibitory concentrations (MIC) values of honey were reported to be less than 11%. Therefore, even when honey diluted by the exudate, it still has potent antibacterial activity .
Regarding systemic antibiotics, the optimal duration of therapy for treating traumatic and implant-related orthopaedic infections remains unclear . It is largely dependent on expert opinion. Rod-Fleury in a study of 49 adults with implant-free chronic osteomyelitis found that a post-debridement antibiotic administration more than 6 weeks did not show increased remission incidences. Benkabouche performed a randomized trial with 123 cases of implant-related osteomyelitis and reported that four weeks duration of antibiotic treatment was not inferior to the currently recommended six weeks after implant removal.
The current study presented chronic wounds of different aetiologies. A wound is considered chronic if its healing is delayed after two to eight weeks. Chronic wound infections are challenging due to the biofilm formation that provide bacterial resistance to antibiotics by extracellular barrier of polymeric substances. Honey is effective in reducing the biofilm of both drug-sensible and drug-resistant strains of Gram-positive and Gram-negative bacteria. Differential gene expression analysis proved the honey ability for down-regulation of several genes related to biofilm formation.
Bacterial resistance to honey has not been reported because of the multiple antimicrobial mechanisms and components working additively and synergistically. This multifactorial nature of honey could explain the wound healing progression in our study despite discontinuation of the initial course of antibiotics administered before complete epithelialisation without any secondary infections.
The present study demonstrated the efficacy of honey on healing of different orthopaedic-related wounds. This dressing method was easy, non-sticky to the wound bed, available and with low cost. The usefulness was demonstrated even with bone and tendon exposure. Undoubtedly, wounds with exposed tendons or bones are serious complications as they are often associated with an increased risk of adverse outcome. This efficacy of honey with exposed tendon and bone could be secondary to the moist hyperosmolar environment and the protective barrier effect which prevent these structures from desiccation in addition to the multifactorial antimicrobial actions. Two single case reports were published and showed the effectiveness and safety after honey dressing. Teobaldi treated a chronic posterior leg ulcer in a diabetic patient with exposed tendon and reported complete epithelisation of more than half of the ulcer after eight weeks and complete tendon coverage after 18 weeks. Astrada presented a diabetic foot ulcer with exposed bone and achieved complete re-epithelialisation after two months of honey dressing. While these reports did not mention any tendon complication, we observed only superficial tendon necrosis. However, the integrity of the remaining most of the tendon persisted.
Conclusion:
With treating the underlying aetiology and optimising the patient’s general condition, honey was an effective, simple and affordable method of infected wound care in different orthopaedic conditions even with exposed bone or tendons. For the proven biological and antibacterial activities, honey has the potential to be new therapeutic choice which should be considered in the clinical orthopaedic practice for infected wound care.
Reference:
He, Haichao, and Zhengliang Zhang. "Honey dressing: a missed way for orthopaedic wound care." International Orthopaedics 46.12 (2022): 2989-2989.





