
BACKGROUND:
Continuous positive airway pressure (CPAP) with nasal devices (nCPAP) is widely used in the respiratory management of newborns. The present study aimed to compare the incidence of nasal trauma secondary to nasal continuous positive airway pressure (nCPAP) protected with or without hydrocolloid dressing in preterm infants.
INTRODUCTION
Continuous positive airway pressure (CPAP) with nasal devices (nCPAP) is widely used in the respiratory management of newborns. nCPAP can improve oxygenation, maintain lung volume, lower upper airway resistance, reduce obstructive apnoea, and most importantly eliminate an ETT/ventilator and the associated risks.A nasal prong is the most commonly used for delivering CPAP because it is less invasive.However, nasal trauma is a well documented complication of noninvasive respiratory support. The local pressure of nasal prongs to the nasal region is easy to cause nasal injury in the newborn due to the cutaneous vulnerability.Besides anatomical factors, such as end-vascularization of the columella and nostrils, Diblasi emphasized that fixation technique was also an important factor for selecting the proper hat and prongs. The lack of stabilization and, hence, excessive movement of the prongs could result in nasal injury, interface displacement, and loss of system pressure. In 2004, Buettiker et al compared three different systems of CPAP: the naso-pharyngeal tube and two-prong systems in newborns, focusing on duration of CPAP, side effects and cost. They found that the naso-pharyngeal tube was an easy, safe and economical CPAP system usable with every common ventilator. For very low birth weight newborns, a prong system may have advantages. In a randomized controlled clinical trial, Yong et al compared the incidence of nasal trauma associated with the use of prong or mask during nCPAP support in very low birthweight (<1 501 g) infants, and reported that there was no significant difference in the incidence of nasal trauma between the two groups (P=0.5). Logistic regression analysis showed that duration of nCPAP was the only significant risk factor associated with development of nasal injury, after birth weight, gestational age, and nasal device used had been controlled. The prolonged use of nCPAP resulted in more pressure, and if there is any area of pressure points exerted by the device, this would definitely cause trauma, no matter what kind of modes. However, injury to the columella during short binasal prongs CPAP had been reported as early as 3 days after CPAP. Yong et alreported an incidence of 35% for nasal trauma in the prongs group. Fischer et al found that 420 (42.5%) of 989 patients developed a nasal trauma. Gunlemez et al demonstrated that the silicon gel on the surface of the nostrils reduced the incidence of nasal injury in preterm infants.
In consideration of hydrocolloid dressing with advantages of an easy to use and cheap, based on the hypothesis that the use of hydrocolloid dressing on the surface of the nostrils could reduce the incidence or severity of nasal injury related to nCPAP used in preterm infants, we conducted a prospective study to investigate the role of hydrocolloid dressing in the prevention of nasal trauma, a common complication of nCPAP in preterm infants.

Figure1: An illustrative case of hydrocolloid dressing with two holes on the nostrils surface of an infant.

Figure 2:Nasal prongs into the nasal cavity of the infant through the holes of hydrocolloid dressing.
METHODS:
This prospective controlled study was performed in the neonatal intensive care unit (NICU) of the Children’s Hospital of Hunan Province from March 1, 2010 to June 31, 2010. A total of 65 infants, 46 males and 19 females, were recruited in this study. Their average gestational age was 32.6 weeks (range 28–37 weeks). The infants were randomly divided into clinical trial group (group A, n=33) and control group (group B, n=32). Paraffin oil was smeared around the nostrils before inserting prongs in group B; the infants in group A were covered on the infant’s nostrils surface with hydrocolloid dressing with a size of 2–3 cm cutting two holes adapted to the nose and nostrils. The nostrils of those infants were inspected daily during nCPAP support until they were weaned off nCPAP.
During the study period of three months, 186 preterm newborns were admitted to the neonatal intensive care unit. A total of 112 premature infants were ventilated with nCPAP. According to the inclusion and exclusion criteria, 65 infants were recruited with 46 males and 19 females in this study. The average gestational age was 32.6 weeks (range 28–37 weeks). The average birth weight was 1 800 g, but 15 neonates were 2 500 g. The underlying diseases included respiratory distress (38 infants), aspiration pneumonia (15 infants), asphyxia (7 infants), and unknown respiratory disease (5 infants).
Nasal injuries were evaluated according to the classification proposed by Buettiker et al, who described the severity of nasal trauma secondary to nCPAP in neonates. Nasal injuries were classified as mild, moderate, and severe. A mild injury was defined as a reddening around the nasal ostium; a moderate injury was defined as bleeding either at the septum or nasal ostium; and a severe nasal injury was defined as necrosis either on the septum or nasal ostium.

Figure : Nasal trauma of mild: erythema around the nostrils with intact skin.

Figure : Columella scar and nasal deformity secondary to columella necrosis at 2 months of age in a premature male infant born at 27+5 weeks of gestational age (birth weight=1 150 g).
Results:
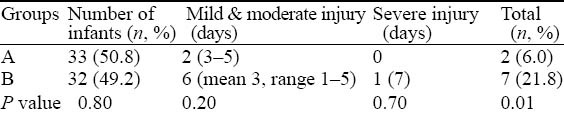
Nine infants (2 in group A and 7 in group B) developed nasal injury during nCPAP support. The Chi-square test revealed that there was a statistically significant difference (P=0.01) in the incidence of nasal injury between groups A and B.
CONCLUSION:
With respect to the management of nasal injury due to nasal CPAP, the optimal recommendation is yet to be established. Yong et al suggested that nCPAP should be terminated as soon as possible. If there was redness, excoriation, or crusting, a protective dressing can be used to prevent worsening. Fischer et al reported that nasal trauma is a frequent complication of nCPAP, especially in preterm neonates, but long-term cosmetic sequelae are very rare. Specific measures like hydrocolloid film and ointment can be used in patients with nasal trauma. Carlisle et al described a novel method of oral CPAP delivery in an extremely premature infant with severe nasal septum erosion. The distal end of a cut down endotracheal tube was passed through a small hole made in the teatment of a dummy (infant pacifier) and sutured in place. The dummy was secured in the infant’s mouth and CPAP was delivered to the pharynx. The device was well tolerated and the infant was successfully managed using this technique for 48 days, avoiding endotracheal intubation and ventilation. In our NICU, mild and moderate nasal injuries were treated by spraying an agent (epidermal growth factor) and hirudoid cream alternatively in order to promote repairment and regeneration of epidermal skin, but nCPAP continued. The severe nasal trauma occurred in one male infant who was CPAP dependent, and treated by oral intubation.
In conclusion, hydrocolloid dressing is a soft, flexible and cheap material, and is easy and safe to use. Preliminary results demonstrated that the incidence and severity of nasal injury such as necrosis of full thickness of skin surrounding the nostrils and columella necrosis significantly decreased. Further study is needed to investigate the efficacy in preterm infants weighing <1 500 g. Meanwhile the short interval (mean 3.2 days) between the initiation of nCPAP and the onset of injury was found, and this suggested that it is necessary to carefully and frequently inspect the nose and nostrils at the first day of application of nCPAP in preterm infants.
KEY WORDS:
Continuous positive airway pressure, Nasal injury, Hydrocolloid dressing, Preterm infants, Nasal prongs.
Reference:
Li-hua. "Hydrocolloid dressing in preventing nasal trauma secondary to nasal continuous positive airway pressure in preterm infants." World journal of emergency medicine 5.3 (2014): 218.





